Hypercholesterolemia
| Hypercholesterolemia | |
|---|---|
| Other names | Hypercholesterolaemia, high cholesterol |
 | |
| A color photograph of two bags of thawed fresh frozen plasma: The bag on the left was obtained from a donor with hypercholesterolemia, and contains altered serum lipid levels, while the bag obtained from a normal donor contains regular serum lipid levels. | |
| Specialty | Cardiology |
| Complications | Atherosclerosis, thrombosis, embolism, heart attack, stroke, coronary thrombosis, fat embolism, cardiovascular and coronary heart disease |
| Causes | Poor diet, junk food, fast food, diabetes, alcoholism, monoclonal gammopathy, dialysis therapy, nephrotic syndrome, hypothyroidism, Cushing's syndrome, anorexia nervosa |
| Differential diagnosis | Hyperlipidemia, hypertriglyceridemia |
Hypercholesterolemia, also called high cholesterol, is the presence of high levels of cholesterol in the blood.[1] It is a form of hyperlipidemia (high levels of lipids in the blood), hyperlipoproteinemia (high levels of lipoproteins in the blood), and dyslipidemia (any abnormalities of lipid and lipoprotein levels in the blood).[1]
Elevated levels of non-HDL cholesterol and LDL in the blood may be a consequence of diet, obesity, inherited (genetic) diseases (such as LDL receptor mutations in familial hypercholesterolemia), or the presence of other diseases such as type 2 diabetes and an underactive thyroid.[1]
Cholesterol is one of three major classes of lipids produced and used by all animal cells to form membranes. Plant cells manufacture phytosterols (similar to cholesterol), but in rather small quantities.[2] Cholesterol is the precursor of the steroid hormones and bile acids. Since cholesterol is insoluble in water, it is transported in the blood plasma within protein particles (lipoproteins). Lipoproteins are classified by their density: very low density lipoprotein (VLDL), intermediate density lipoprotein (IDL), low density lipoprotein (LDL) and high density lipoprotein (HDL).[3] All the lipoproteins carry cholesterol, but elevated levels of the lipoproteins other than HDL (termed non-HDL cholesterol), particularly LDL-cholesterol, are associated with an increased risk of atherosclerosis and coronary heart disease.[4] In contrast, higher levels of HDL cholesterol are protective.[5]
Avoiding trans fats and replacing saturated fats in adult diets with polyunsaturated fats are recommended dietary measures to reduce total blood cholesterol and LDL in adults.[6][7] In people with very high cholesterol (e.g., familial hypercholesterolemia), diet is often not sufficient to achieve the desired lowering of LDL, and lipid-lowering medications are usually required.[8] If necessary, other treatments such as LDL apheresis or even surgery (for particularly severe subtypes of familial hypercholesterolemia) are performed.[8] About 34 million adults in the United States have high blood cholesterol.[9]
Signs and symptoms
[edit]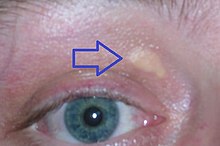
Although hypercholesterolemia itself is asymptomatic, longstanding elevation of serum cholesterol can lead to atherosclerosis (build-up of fatty plaques in the arteries, so-called 'hardening of the arteries').[10] Over a period of decades, elevated serum cholesterol contributes to formation of atheromatous plaques in the arteries. This can lead to progressive narrowing of the involved arteries. Alternatively smaller plaques may rupture and cause a clot to form and obstruct blood flow.[11] A sudden blockage of a coronary artery may result in a heart attack. A blockage of an artery supplying the brain can cause a stroke. If the development of the stenosis or occlusion is gradual, blood supply to the tissues and organs slowly diminishes until organ function becomes impaired. At this point tissue ischemia (restriction in blood supply) may manifest as specific symptoms. For example, temporary ischemia of the brain (commonly referred to as a transient ischemic attack) may manifest as temporary loss of vision, dizziness and impairment of balance, difficulty speaking, weakness or numbness or tingling, usually on one side of the body. Insufficient blood supply to the heart may cause chest pain, and ischemia of the eye may manifest as transient visual loss in one eye. Insufficient blood supply to the legs may manifest as calf pain when walking, while in the intestines it may present as abdominal pain after eating a meal.[1][12]
Some types of hypercholesterolemia lead to specific physical findings. For example, familial hypercholesterolemia (Type IIa hyperlipoproteinemia) may be associated with xanthelasma palpebrarum (yellowish patches underneath the skin around the eyelids),[13] arcus senilis (white or gray discoloration of the peripheral cornea),[14] and xanthomata (deposition of yellowish cholesterol-rich material) of the tendons, especially of the fingers.[15][16] Type III hyperlipidemia may be associated with xanthomata of the palms, knees and elbows.[15]
Causes
[edit]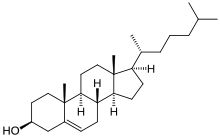
Hypercholesterolemia is typically due to a combination of environmental and genetic factors.[10] Environmental factors include weight, diet, and stress.[10][17] Loneliness is also a risk factor.[18]
Diet
[edit]Diet has an effect on blood cholesterol, but the size of this effect varies between individuals.[19][20]
A diet high in sugar or saturated fats increases total cholesterol and LDL.[21] Trans fats have been shown to reduce levels of high-density lipoprotein while increasing levels of LDL.[22]
A 2016 review found tentative evidence that dietary cholesterol is associated with higher blood cholesterol.[23] As of 2018 there appears to be a modest positive, dose-related relationship between cholesterol intake and LDL cholesterol.[24]
Medical conditions and treatments
[edit]A number of other conditions can also increase cholesterol levels including diabetes mellitus type 2, obesity, alcohol use, monoclonal gammopathy, dialysis therapy, nephrotic syndrome, hypothyroidism, Cushing's syndrome and anorexia nervosa.[10] Several medications and classes of medications may interfere with lipid metabolism: thiazide diuretics, ciclosporin, glucocorticoids, beta blockers, retinoic acid, antipsychotics,[10] certain anticonvulsants and medications for HIV as well as interferons.[25]
Genetics
[edit]Genetic contributions typically arise from the combined effects of multiple genes, known as "polygenic," although in certain cases, they may stem from a single gene defect, as seen in familial hypercholesterolemia.[10] In familial hypercholesterolemia, mutations may be present in the APOB gene (autosomal dominant), the autosomal recessive LDLRAP1 gene, autosomal dominant familial hypercholesterolemia (HCHOLA3) variant of the PCSK9 gene, or the LDL receptor gene.[26] Familial hypercholesterolemia affects about one in 250 individuals.[27]
The Lithuanian Jewish population may exhibit a genetic founder effect.[28] One variation, G197del LDLR which is implicated in familial hypercholesterolemia, has been dated to the 14th century.[29] The utility[clarification needed] of these variations has been the subject of debate.[30]
Diagnosis
[edit]| Cholesterol type | mmol/L | mg/dL | Interpretation |
|---|---|---|---|
| total cholesterol | <5.2 | <200 | Desirable[31] |
| 5.2–6.2 | 200–239 | Borderline[31] | |
| >6.2 | >240 | High[31] | |
| LDL cholesterol | <2.6 | <100 | Most desirable[31] |
| 2.6–3.3 | 100–129 | Good[31] | |
| 3.4–4.1 | 130–159 | Borderline high[31] | |
| 4.1–4.9 | 160–189 | High and undesirable[31] | |
| >4.9 | >190 | Very high[31] | |
| HDL cholesterol | <1.0 | <40 | Undesirable; risk increased[31] |
| 1.0–1.5 | 41–59 | Okay, but not optimal[31] | |
| >1.55 | >60 | Good; risk lowered[31] |
Cholesterol is measured in milligrams per deciliter (mg/dL) of blood in the United States and some other countries. In the United Kingdom, most European countries and Canada, millimoles per liter of blood (mmol/L) is the measure.[32]
For healthy adults, the UK National Health Service recommends upper limits of total cholesterol of 5 mmol/L, and low-density lipoprotein cholesterol (LDL) of 3 mmol/L. For people at high risk of cardiovascular disease, the recommended limit for total cholesterol is 4 mmol/L, and 2 mmol/L for LDL.[33]
In the United States, the National Heart, Lung, and Blood Institute within the National Institutes of Health classifies total cholesterol of less than 200 mg/dL as "desirable", 200 to 239 mg/dL as "borderline high", and 240 mg/dL or more as "high".[34]
There is no absolute cutoff between normal and abnormal cholesterol levels, and values must be considered in relation to other health conditions and risk factors.[35][36][37]
Higher levels of total cholesterol increase the risk of cardiovascular disease, particularly coronary heart disease.[38] Levels of LDL or non-HDL cholesterol both predict future coronary heart disease; which is the better predictor is disputed.[39] High levels of small dense LDL may be particularly adverse, although measurement of small dense LDL is not advocated for risk prediction.[39] In the past, LDL and VLDL levels were rarely measured directly due to cost.[40][41][42]
Levels of fasting triglycerides were taken as an indicator of VLDL levels (generally about 45% of fasting triglycerides is composed of VLDL), while LDL was usually estimated by the Friedewald formula:
LDL total cholesterol – HDL – (0.2 x fasting triglycerides).[43]
However, this equation is not valid on nonfasting blood samples or if fasting triglycerides are elevated (>4.5 mmol/L or >~400 mg/dL). Recent guidelines have, therefore, advocated the use of direct methods for measurement of LDL wherever possible.[39] It may be useful to measure all lipoprotein subfractions (VLDL, IDL, LDL, and HDL) when assessing hypercholesterolemia and measurement of apolipoproteins and lipoprotein (a) can also be of value.[39] Genetic screening is now advised if a form of familial hypercholesterolemia is suspected.[39]
Classification
[edit]Classically, hypercholesterolemia was categorized by lipoprotein electrophoresis and the Fredrickson classification. Newer methods, such as "lipoprotein subclass analysis", have offered significant improvements in understanding the connection with atherosclerosis progression and clinical consequences. If the hypercholesterolemia is hereditary (familial hypercholesterolemia), more often a family history of premature, earlier onset atherosclerosis is found.[44]
Screening method
[edit]The U.S. Preventive Services Task Force in 2008 strongly recommends routine screening for men 35 years and older and women 45 years and older for lipid disorders and the treatment of abnormal lipids in people who are at increased risk of coronary heart disease. They also recommend routinely screening men aged 20 to 35 years and women aged 20 to 45 years if they have other risk factors for coronary heart disease.[45] In 2016 they concluded that testing the general population under the age of 40 without symptoms is of unclear benefit.[46][47]
In Canada, screening is recommended for men 40 and older and women 50 and older.[48] In those with normal cholesterol levels, screening is recommended once every five years.[49] Once people are on a statin further testing provides little benefit except possibly to determine compliance with treatment.[50]
In the UK, after someone is diagnosed with familial hypercholesterolemia, clinicians, family, or both, contact first- and second-degree relatives to come forward for testing and treatment. Research suggests that clinician-only contact results in more people coming forward for testing.[51][52]
Treatment
[edit]Treatment recommendations have been based on four risk levels for heart disease.[53] For each risk level, LDL cholesterol levels representing goals and thresholds for treatment and other action are made.[53] The higher the risk category, the lower the cholesterol thresholds.[53]
| Risk category | Criteria for risk category | Consider lifestyle modifications | Consider medication | ||||
|---|---|---|---|---|---|---|---|
| No. of risk factors† | 10-year risk of myocardial ischemia |
mmol/litre | mg/dL | mmol/litre | mg/dL | ||
| High | Prior heart disease | OR | >20% | >2.6[54] | >100 | >2.6 | >100 |
| Moderately high | 2 or more | AND | 10–20% | >3.4 | >130 | >3.4 | >130 |
| Moderate | 2 or more | AND | <10% | >3.4 | >130 | >4.1 | >160 |
| Low | 0 or 1 | >4.1 | >160 | >4.9 | >190 | ||
| †Risk factors include cigarette smoking, hypertension (BP ≥140/90 mm Hg or on antihypertensive medication), low HDL cholesterol (<40 mg/dL), family history of premature heart disease, and age (men ≥45 years; women ≥55 years). | |||||||
For those at high risk, a combination of lifestyle modification and statins has been shown to decrease mortality.[10]
Lifestyle
[edit]Lifestyle changes recommended for those with high cholesterol include: smoking cessation, limiting alcohol consumption, increasing physical activity, and maintaining a healthy weight.[19]
Overweight or obese individuals can lower blood cholesterol by losing weight – on average a kilogram of weight loss can reduce LDL cholesterol by 0.8 mg/dl.[8]
Diet
[edit]Eating a diet with a high proportion of vegetables, fruit, dietary fibre, and low in fats results in a modest decrease in total cholesterol.[55][56][8]
Eating dietary cholesterol causes a small rise in serum cholesterol,[57][58] the magnitude of which can be predicted using the Keys[59] and Hegsted[60] equations. Dietary limits for cholesterol were proposed in United States, but not in Canada, United Kingdom, and Australia.[57] However, in 2015 the Dietary Guidelines Advisory Committee in the United States removed its recommendation of limiting cholesterol intake.[61]
A 2020 Cochrane review found replacing saturated fat with polyunsaturated fat resulted in a small decrease in cardiovascular disease by decreasing blood cholesterol.[62] Other reviews have not found an effect from saturated fats on cardiovascular disease.[63][7] Trans fats are recognized as a potential risk factor for cholesterol-related cardiovascular disease, and avoiding them in an adult diet is recommended.[7]
The National Lipid Association recommends that people with familial hypercholesterolemia restrict intakes of total fat to 25–35% of energy intake, saturated fat to less than 7% of energy intake, and cholesterol to less than 200 mg per day.[8] Changes in total fat intake in low calorie diets do not appear to affect blood cholesterol.[64]
Increasing soluble fiber consumption has been shown to reduce levels of LDL cholesterol, with each additional gram of soluble fiber reducing LDL by an average of 2.2 mg/dL (0.057 mmol/L).[65] Increasing consumption of whole grains also reduces LDL cholesterol, with whole grain oats being particularly effective.[66] Inclusion of 2 g per day of phytosterols and phytostanols and 10 to 20 g per day of soluble fiber decreases dietary cholesterol absorption.[8] A diet high in fructose can raise LDL cholesterol levels in the blood.[67]
Medication
[edit]Statins are the typically used medications, in addition to healthy lifestyle interventions.[68] Statins can reduce total cholesterol by about 50% in the majority of people,[39] and are effective in reducing the risk of cardiovascular disease in both people with[69] and without pre-existing cardiovascular disease.[70][71][72][73] In people without cardiovascular disease, statins have been shown to reduce all-cause mortality, fatal and non-fatal coronary heart disease, and strokes.[74] Greater benefit is observed with the use of high-intensity statin therapy.[75] Statins may improve quality of life when used in people without existing cardiovascular disease (i.e. for primary prevention).[74] Statins decrease cholesterol in children with hypercholesterolemia, but no studies as of 2010 show improved outcomes[76] and diet is the mainstay of therapy in childhood.[39]
Other agents that may be used include fibrates, nicotinic acid, and cholestyramine.[77] These, however, are only recommended if statins are not tolerated or in pregnant women.[77] Injectable antibodies against the protein PCSK9 (evolocumab, bococizumab, alirocumab) can reduce LDL cholesterol and have been shown to reduce mortality.[78]
Guidelines
[edit]In the US, guidelines exist from the National Cholesterol Education Program (2004)[79] and a joint body of professional societies led by the American Heart Association.[80]
In the UK, the National Institute for Health and Clinical Excellence has made recommendations for the treatment of elevated cholesterol levels, published in 2008,[77] and a new guideline appeared in 2014 that covers the prevention of cardiovascular disease in general.[81]
The Task Force for the management of dyslipidaemias of the European Society of Cardiology and the European Atherosclerosis Society published guidelines for the management of dyslipidaemias in 2011.[39]
Specific populations
[edit]Among people whose life expectancy is relatively short, hypercholesterolemia is not a risk factor for death by any cause including coronary heart disease.[82] Among people older than 70, hypercholesterolemia is not a risk factor for being hospitalized with myocardial infarction or angina.[82] There are also increased risks in people older than 85 in the use of statin drugs.[82] Because of this, medications which lower lipid levels should not be routinely used among people with limited life expectancy.[82]
The American College of Physicians recommends for hypercholesterolemia in people with diabetes:[83]
- Lipid-lowering therapy should be used for secondary prevention of cardiovascular mortality and morbidity for all adults with known coronary artery disease and type 2 diabetes.
- Statins should be used for primary prevention against macrovascular (coronary artery disease, cerebrovascular disease, or peripheral vascular disease) complications in adults with type 2 diabetes and other cardiovascular risk factors.
- Once lipid-lowering therapy is initiated, people with type 2 diabetes mellitus should be taking at least moderate doses of a statin.[84]
- For those people with type 2 diabetes who are taking statins, routine monitoring of liver function tests or muscle enzymes is not recommended except in specific circumstances.
Alternative medicine
[edit]A 2002 survey found that 1.1% of U.S. adults who used alternative medicine did so to treat high cholesterol. Consistent with previous surveys, this one found the majority of individuals (55%) used it in conjunction with conventional medicine.[85] A systematic review[86] of the effectiveness of herbal medicines used in traditional Chinese medicine had inconclusive results due to the poor methodological quality of the included studies. A review of trials of phytosterols and/or phytostanols, average dose 2.15 g/day, reported an average of 9% lowering of LDL-cholesterol.[87] In 2000, the Food and Drug Administration approved the labeling of foods containing specified amounts of phytosterol esters or phytostanol esters as cholesterol-lowering; in 2003, an FDA Interim Health Claim Rule extended that label claim to foods or dietary supplements delivering more than 0.8 g/day of phytosterols or phytostanols. Some researchers, however, are concerned about diet supplementation with plant sterol esters and draw attention to lack of long-term safety data.[88]
Epidemiology
[edit]Rates of high total cholesterol in the United States in 2010 are just over 13%, down from 17% in 2000.[89]
Average total cholesterol in the United Kingdom is 5.9 mmol/L, while in rural China and Japan, average total cholesterol is 4 mmol/L.[10] Rates of coronary artery disease are high in Great Britain, but low in rural China and Japan.[10]
Research directions
[edit]Gene therapy is being studied as a potential treatment.[90][91]
References
[edit]- ^ a b c d Durrington P (August 2003). "Dyslipidaemia". Lancet. 362 (9385): 717–731. doi:10.1016/S0140-6736(03)14234-1. PMID 12957096. S2CID 208792416.
- ^ Behrman EJ, Gopalan V (December 2005). "Cholesterol and Plants". Journal of Chemical Education. 82 (12): 1791. Bibcode:2005JChEd..82.1791B. doi:10.1021/ed082p1791. ISSN 0021-9584.
- ^ Biggerstaff KD, Wooten JS (December 2004). "Understanding lipoproteins as transporters of cholesterol and other lipids". Advances in Physiology Education. 28 (1–4): 105–106. doi:10.1152/advan.00048.2003. PMID 15319192. S2CID 30197456.
- ^ Carmena R, Duriez P, Fruchart JC (June 2004). "Atherogenic lipoprotein particles in atherosclerosis". Circulation. 109 (23 Suppl 1): III2–III7. doi:10.1161/01.CIR.0000131511.50734.44. PMID 15198959.
- ^ Kontush A, Chapman MJ (March 2006). "Antiatherogenic small, dense HDL--guardian angel of the arterial wall?". Nature Clinical Practice. Cardiovascular Medicine. 3 (3): 144–153. doi:10.1038/ncpcardio0500. PMID 16505860. S2CID 27738163.
- ^ "Healthy diet – Fact sheet N°394". World Health Organization. September 2015. Retrieved July 6, 2016.
- ^ a b c de Souza RJ, Mente A, Maroleanu A, Cozma AI, Ha V, Kishibe T, et al. (August 2015). "Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: systematic review and meta-analysis of observational studies". BMJ. 351: h3978. doi:10.1136/bmj.h3978. PMC 4532752. PMID 26268692.
- ^ a b c d e f Ito MK, McGowan MP, Moriarty PM (June 2011). "Management of familial hypercholesterolemias in adult patients: recommendations from the National Lipid Association Expert Panel on Familial Hypercholesterolemia". Journal of Clinical Lipidology. 5 (3 Suppl): S38–S45. doi:10.1016/j.jacl.2011.04.001. PMID 21600528.
- ^ "Hypercholesterolemia". Genetics Home Reference. Retrieved 16 May 2016.
- ^ a b c d e f g h i Bhatnagar D, Soran H, Durrington PN (August 2008). "Hypercholesterolaemia and its management". BMJ. 337: a993. doi:10.1136/bmj.a993. PMID 18719012. S2CID 5339837.
- ^ Finn AV, Nakano M, Narula J, Kolodgie FD, Virmani R (July 2010). "Concept of vulnerable/unstable plaque". Arteriosclerosis, Thrombosis, and Vascular Biology. 30 (7): 1282–1292. doi:10.1161/ATVBAHA.108.179739. PMID 20554950.
- ^ Grundy SM, Balady GJ, Criqui MH, Fletcher G, Greenland P, Hiratzka LF, et al. (May 1998). "Primary prevention of coronary heart disease: guidance from Framingham: a statement for healthcare professionals from the AHA Task Force on Risk Reduction. American Heart Association". Circulation. 97 (18): 1876–1887. doi:10.1161/01.CIR.97.18.1876. PMID 9603549.
- ^ Shields C, Shields J (2008). Eyelid, conjunctival, and orbital tumors: atlas and textbook. Hagerstown, Maryland: Lippincott Williams & Wilkins. ISBN 978-0-7817-7578-6.
- ^ Zech LA, Hoeg JM (March 2008). "Correlating corneal arcus with atherosclerosis in familial hypercholesterolemia". Lipids in Health and Disease. 7 (1): 7. doi:10.1186/1476-511X-7-7. PMC 2279133. PMID 18331643.
- ^ a b James WD, Berger TG (2006). Andrews' Diseases of the Skin: Clinical Dermatology. Saunders Elsevier. pp. 530–32. ISBN 978-0-7216-2921-6.
- ^ Rapini RP, Bolognia JL, Jorizzo JL (2007). Dermatology: 2-Volume Set. St. Louis, Missouri: Mosby. pp. 1415–16. ISBN 978-1-4160-2999-1.
- ^ Calderon R, Schneider RH, Alexander CN, Myers HF, Nidich SI, Haney C (1999). "Stress, stress reduction and hypercholesterolemia in African Americans: a review". Ethnicity & Disease. 9 (3): 451–62. PMID 10600068.
- ^ Hawkley LC, Cacioppo JT (October 2010). "Loneliness matters: a theoretical and empirical review of consequences and mechanisms". Annals of Behavioral Medicine. 40 (2): 218–227. doi:10.1007/s12160-010-9210-8. PMC 3874845. PMID 20652462.
- ^ a b Mannu GS, Zaman MJ, Gupta A, Rehman HU, Myint PK (February 2013). "Evidence of lifestyle modification in the management of hypercholesterolemia". Current Cardiology Reviews. 9 (1): 2–14. doi:10.2174/157340313805076313. PMC 3584303. PMID 22998604.
- ^ Howell WH, McNamara DJ, Tosca MA, Smith BT, Gaines JA (June 1997). "Plasma lipid and lipoprotein responses to dietary fat and cholesterol: a meta-analysis". The American Journal of Clinical Nutrition. 65 (6): 1747–1764. doi:10.1093/ajcn/65.6.1747. PMID 9174470.
- ^ DiNicolantonio JJ, Lucan SC, O'Keefe JH (2016). "The Evidence for Saturated Fat and for Sugar Related to Coronary Heart Disease". Progress in Cardiovascular Diseases. 58 (5): 464–472. doi:10.1016/j.pcad.2015.11.006. PMC 4856550. PMID 26586275.
- ^ Ascherio A, Willett WC (October 1997). "Health effects of trans fatty acids". The American Journal of Clinical Nutrition. 66 (4 Suppl): 1006S–1010S. doi:10.1093/ajcn/66.4.1006S. PMID 9322581.
- ^ Grundy SM (November 2016). "Does Dietary Cholesterol Matter?". Current Atherosclerosis Reports. 18 (11): 68. doi:10.1007/s11883-016-0615-0. PMID 27739004. S2CID 30969287.
- ^ Vincent MJ, Allen B, Palacios OM, Haber LT, Maki KC (January 2019). "Meta-regression analysis of the effects of dietary cholesterol intake on LDL and HDL cholesterol". The American Journal of Clinical Nutrition. 109 (1): 7–16. doi:10.1093/ajcn/nqy273. PMID 30596814.
- ^ Herink M, Ito MK (2000-01-01). "Medication Induced Changes in Lipid and Lipoproteins". In De Groot LJ, Chrousos G, Dungan K, Feingold KR, Grossman A, Hershman JM, Koch C, Korbonits M, McLachlan R (eds.). Endotext. South Dartmouth (MA): MDText.com, Inc. PMID 26561699.
- ^ "Hypercholesterolemia". Genetics Home Reference. U.S. National Institutes of Health. Retrieved 5 December 2013.
- ^ Akioyamen LE, Genest J, Shan SD, Reel RL, Albaum JM, Chu A, Tu JV (September 2017). "Estimating the prevalence of heterozygous familial hypercholesterolaemia: a systematic review and meta-analysis". BMJ Open. 7 (9): e016461. doi:10.1136/bmjopen-2017-016461. PMC 5588988. PMID 28864697.
- ^ Slatkin, M (August 2004). "A Population-Genetic Test of Founder Effects and Implications for Ashkenazi Jewish Diseases". Am. J. Hum. Genet. 75 (2). American Society of Human Genetics via PubMed: 282–93. doi:10.1086/423146. PMC 1216062. PMID 15208782.
- ^ Durst, Ronen (May 2001), "Recent Origin and Spread of a Common Lithuanian Mutation, G197del LDLR, Causing Familial Hypercholesterolemia: Positive Selection Is Not Always Necessary to Account for Disease Incidence among Ashkenazi Jews", American Journal of Human Genetics, 68 (5), Roberto Colombo, Shoshi Shpitzen, Liat Ben Avi, et al.: 1172–1188, doi:10.1086/320123, PMC 1226098, PMID 11309683
- ^ "Jewish Genetics, Part 3: Jewish Genetic Diseases (Mediterranean Fever, Tay–Sachs, pemphigus vulgaris, Mutations)". www.khazaria.com. Retrieved 18 October 2018.
- ^ a b c d e f g h i j k Consumer Reports; Drug Effectiveness Review Project (March 2013). "Evaluating statin drugs to treat High Cholesterol and Heart Disease: Comparing Effectiveness, Safety, and Price" (PDF). Best Buy Drugs. Consumer Reports: 9. Retrieved 27 March 2013. which cites
- United States Department of Health and Human Services; National Heart Lung and Blood Institute; National Institutes of Health (June 2005). "NHLBI, High Blood Cholesterol: What You Need to Know". nhlbi.nih.gov. Archived from the original on 1 April 2013. Retrieved 27 March 2013.
- ^ "Diagnosis and treatment". Mayo Clinic. 2023-01-11. Archived from the original on 2024-03-13. Retrieved 2024-03-16.
- ^ Diagnosing High Cholesterol, NHS Choices. Retrieved 2013-03-09.
- ^ ATP III Guidelines At-A-Glance Quick Desk Reference, National Cholesterol Education Program. Retrieved 2013-03-09.
- ^
Davidson, Michael H.; Pradeep, Pallavi (2023-07-03). "Hormonal and Metabolic Disorders". MSD Manual Consumer Version. Archived from the original on 2023-11-14. Retrieved 2024-03-16.
Although there is no natural cutoff between normal and abnormal cholesterol levels, ...
- ^
"What Your Cholesterol Levels Mean". www.heart.org. 2017-11-16. Archived from the original on 2024-02-26. Retrieved 2024-03-16.
While cholesterol levels above "normal ranges" are important in your overall cardiovascular risk, like HDL and LDL cholesterol levels, your total blood cholesterol level should be considered in context with your other known risk factors.
- ^
Nantsupawat, Nopakoon; Booncharoen, Apaputch; Wisetborisut, Anawat; Jiraporncharoen, Wichuda; et al. (2019-01-26). "Appropriate Total cholesterol cut-offs for detection of abnormal LDL cholesterol and non-HDL cholesterol among low cardiovascular risk population". Lipids in Health and Disease. 18 (1): 28. doi:10.1186/s12944-019-0975-x. ISSN 1476-511X. PMC 6347761. PMID 30684968.
The current appropriate TC cutoff to determine whether patients need further investigation and assessment is between 200 and 240 mg/dL [1, 17, 18]. However, the appropriate cut-off point for the younger population who may have low cardiovascular risk have not been examined extensively in the literature. A recent study suggests that a TC cut of point of between 200 and 240 may not be appropriate in identifying high LDL-C levels in apparently healthy people.
- ^ Peters SA, Singhateh Y, Mackay D, Huxley RR, Woodward M (May 2016). "Total cholesterol as a risk factor for coronary heart disease and stroke in women compared with men: A systematic review and meta-analysis". Atherosclerosis. 248: 123–131. doi:10.1016/j.atherosclerosis.2016.03.016. PMID 27016614.
- ^ a b c d e f g h Reiner Z, Catapano AL, De Backer G, Graham I, Taskinen MR, Wiklund O, et al. (July 2011). "ESC/EAS Guidelines for the management of dyslipidaemias: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS)". European Heart Journal. 32 (14): 1769–1818. doi:10.1093/eurheartj/ehr158. PMID 21712404.
- ^ Superko, H. Robert (2009-05-05). "Advanced Lipoprotein Testing and Subfractionation Are Clinically Useful". Circulation. 119 (17): 2383–2395. doi:10.1161/CIRCULATIONAHA.108.809582. ISSN 0009-7322. PMID 19414656.
- ^ "New Information on Accuracy of LDL-C Estimation". American College of Cardiology. 2020-03-20. Archived from the original on 2023-12-06. Retrieved 2024-03-16.
- ^ "Friedewald equation for calculating VLDL and LDL - All About Cardiovascular System and Disorders". Johnson's Techworld - Reliving my hobbies. 2017-11-04. Archived from the original on 2023-09-28. Retrieved 2024-03-16.
- ^ Friedewald WT, Levy RI, Fredrickson DS (June 1972). "Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge". Clinical Chemistry. 18 (6): 499–502. doi:10.1093/clinchem/18.6.499. PMID 4337382.
- ^ Ison HE, Clarke SL, Knowles JW (1993). "Familial Hypercholesterolemia". In Adam MP, Ardinger HH, Pagon RA, Wallace SE (eds.). GeneReviews. Seattle (WA): University of Washington, Seattle. PMID 24404629. Retrieved 2021-01-04.
- ^ U.S. Preventive Services Task Force. "Screening for Lipid Disorders: Recommendations and Rationale". Archived from the original on 2015-02-10. Retrieved 2010-11-04.
- ^ Chou R, Dana T, Blazina I, Daeges M, Bougatsos C, Jeanne TL (October 2016). "Screening for Dyslipidemia in Younger Adults: A Systematic Review for the U.S. Preventive Services Task Force". Annals of Internal Medicine. 165 (8): 560–564. doi:10.7326/M16-0946. PMID 27538032. S2CID 20592431.
- ^ Bibbins-Domingo K, Grossman DC, Curry SJ, Davidson KW, Epling JW, García FA, et al. (August 2016). "Screening for Lipid Disorders in Children and Adolescents: US Preventive Services Task Force Recommendation Statement". JAMA. 316 (6): 625–633. doi:10.1001/jama.2016.9852. PMID 27532917.
- ^ Genest J, Frohlich J, Fodor G, McPherson R (October 2003). "Recommendations for the management of dyslipidemia and the prevention of cardiovascular disease: summary of the 2003 update". CMAJ. 169 (9): 921–924. PMC 219626. PMID 14581310.
- ^ "Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report". Circulation. 106 (25): 3143–3421. December 2002. doi:10.1161/circ.106.25.3143. hdl:2027/uc1.c095473168. PMID 12485966.
- ^ Spector R, Snapinn SM (2011). "Statins for secondary prevention of cardiovascular disease: the right dose". Pharmacology. 87 (1–2): 63–69. doi:10.1159/000322999. PMID 21228612.
- ^ Qureshi, Nadeem; Woods, Bethan; Neves de Faria, Rita; Saramago Goncalves, Pedro; Cox, Edward; Leonardi-Bee, Jo; Condon, Laura; Weng, Stephen; Akyea, Ralph K.; Iyen, Barbara; Roderick, Paul; Humphries, Steve E.; Rowlands, William; Watson, Melanie; Haralambos, Kate (2023-10-24). "Alternative cascade-testing protocols for identifying and managing patients with familial hypercholesterolaemia: systematic reviews, qualitative study and cost-effectiveness analysis". Health Technology Assessment. 27 (16): 1–140. doi:10.3310/CTMD0148. ISSN 2046-4924. PMC 10658348. PMID 37924278.
- ^ "What is the best way to identify people with inherited high cholesterol?". NIHR Evidence. 30 April 2024. doi:10.3310/nihrevidence_62958.
- ^ a b c d Grundy SM, Cleeman JI, Merz CN, Brewer HB, Clark LT, Hunninghake DB, et al. (July 2004). "Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines". Circulation. 110 (2): 227–239. doi:10.1161/01.cir.0000133317.49796.0e. PMID 15249516.
- ^ Consumer Reports; Drug Effectiveness Review Project (March 2013). "Evaluating statin drugs to treat High Cholesterol and Heart Disease: Comparing Effectiveness, Safety, and Price" (PDF). Best Buy Drugs. Consumer Reports: 9. Retrieved 27 March 2013.
- ^ Bhattarai N, Prevost AT, Wright AJ, Charlton J, Rudisill C, Gulliford MC (December 2013). "Effectiveness of interventions to promote healthy diet in primary care: systematic review and meta-analysis of randomised controlled trials". BMC Public Health. 13: 1203. doi:10.1186/1471-2458-13-1203. PMC 3890643. PMID 24355095.
- ^ Hartley L, Igbinedion E, Holmes J, Flowers N, Thorogood M, Clarke A, et al. (June 2013). "Increased consumption of fruit and vegetables for the primary prevention of cardiovascular diseases". The Cochrane Database of Systematic Reviews. 2013 (6): CD009874. doi:10.1002/14651858.CD009874.pub2. PMC 4176664. PMID 23736950.
- ^ a b Brownawell AM, Falk MC (June 2010). "Cholesterol: where science and public health policy intersect". Nutrition Reviews. 68 (6): 355–364. doi:10.1111/j.1753-4887.2010.00294.x. PMID 20536780.
- ^ Berger S, Raman G, Vishwanathan R, Jacques PF, Johnson EJ (August 2015). "Dietary cholesterol and cardiovascular disease: a systematic review and meta-analysis". The American Journal of Clinical Nutrition. 102 (2): 276–294. doi:10.3945/ajcn.114.100305. PMID 26109578.
- ^ Keys A, Anderson JT, Grande F (July 1965). "Serum cholesterol response to changes in the diet: IV. Particular saturated fatty acids in the diet". Metabolism. 14 (7): 776–787. doi:10.1016/0026-0495(65)90004-1. PMID 25286466.
- ^ Hegsted DM, McGandy RB, Myers ML, Stare FJ (November 1965). "Quantitative effects of dietary fat on serum cholesterol in man". The American Journal of Clinical Nutrition. 17 (5): 281–295. doi:10.1093/ajcn/17.5.281. PMID 5846902.
- ^ "Scientific Report of the 2015 Dietary Guidelines Advisory Committee" (PDF). health.gov. 2015. p. 17. Retrieved 16 May 2016.
The 2015 DGAC will not bring forward this recommendation 644 because available evidence shows no appreciable relationship between consumption of dietary cholesterol and serum cholesterol, consistent with the conclusions of the AHA/ACC report.
- ^ Hooper L, Martin N, Jimoh OF, Kirk C, Foster E, Abdelhamid AS (August 2020). "Reduction in saturated fat intake for cardiovascular disease". The Cochrane Database of Systematic Reviews. 2020 (8): CD011737. doi:10.1002/14651858.CD011737.pub3. PMC 8092457. PMID 32827219.
- ^ Chowdhury R, Warnakula S, Kunutsor S, Crowe F, Ward HA, Johnson L, et al. (March 2014). "Association of dietary, circulating, and supplement fatty acids with coronary risk: a systematic review and meta-analysis". Annals of Internal Medicine. 160 (6): 398–406. doi:10.7326/M13-1788. PMID 24723079.
- ^ Schwingshackl L, Hoffmann G (December 2013). "Comparison of effects of long-term low-fat vs high-fat diets on blood lipid levels in overweight or obese patients: a systematic review and meta-analysis". Journal of the Academy of Nutrition and Dietetics. 113 (12): 1640–1661. doi:10.1016/j.jand.2013.07.010. PMID 24139973.
Including only hypocaloric diets, the effects of low-fat vs high-fat diets on total cholesterol and LDL cholesterol levels were abolished.
- ^ Brown L, Rosner B, Willett WW, Sacks FM (January 1999). "Cholesterol-lowering effects of dietary fiber: a meta-analysis". The American Journal of Clinical Nutrition. 69 (1): 30–42. doi:10.1093/ajcn/69.1.30. PMID 9925120.
- ^ Hollænder PL, Ross AB, Kristensen M (September 2015). "Whole-grain and blood lipid changes in apparently healthy adults: a systematic review and meta-analysis of randomized controlled studies". The American Journal of Clinical Nutrition. 102 (3): 556–572. doi:10.3945/ajcn.115.109165. PMID 26269373.
- ^ Schaefer EJ, Gleason JA, Dansinger ML (June 2009). "Dietary fructose and glucose differentially affect lipid and glucose homeostasis". The Journal of Nutrition. 139 (6): 1257S–1262S. doi:10.3945/jn.108.098186. PMC 2682989. PMID 19403705.
- ^ Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. (June 2019). "2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines". Circulation. 139 (25): e1082–e1143. doi:10.1161/CIR.0000000000000625. PMC 7403606. PMID 30586774.
- ^ Koskinas KC, Siontis GC, Piccolo R, Mavridis D, Räber L, Mach F, Windecker S (April 2018). "Effect of statins and non-statin LDL-lowering medications on cardiovascular outcomes in secondary prevention: a meta-analysis of randomized trials". European Heart Journal. 39 (14): 1172–1180. doi:10.1093/eurheartj/ehx566. PMID 29069377.
- ^ Tonelli M, Lloyd A, Clement F, Conly J, Husereau D, Hemmelgarn B, et al. (November 2011). "Efficacy of statins for primary prevention in people at low cardiovascular risk: a meta-analysis". CMAJ. 183 (16): E1189–E1202. doi:10.1503/cmaj.101280. PMC 3216447. PMID 21989464.
- ^ Mills EJ, Wu P, Chong G, Ghement I, Singh S, Akl EA, et al. (February 2011). "Efficacy and safety of statin treatment for cardiovascular disease: a network meta-analysis of 170,255 patients from 76 randomized trials". QJM. 104 (2): 109–124. doi:10.1093/qjmed/hcq165. PMID 20934984.
- ^ Mihaylova B, Emberson J, Blackwell L, Keech A, Simes J, Barnes EH, et al. (Cholesterol Treatment Trialists' Collaborators) (August 2012). "The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials". Lancet. 380 (9841): 581–590. doi:10.1016/S0140-6736(12)60367-5. PMC 3437972. PMID 22607822.
- ^ Chou R, Dana T, Blazina I, Daeges M, Jeanne TL (November 2016). "Statins for Prevention of Cardiovascular Disease in Adults: Evidence Report and Systematic Review for the US Preventive Services Task Force". JAMA. 316 (19): 2008–2024. doi:10.1001/jama.2015.15629. PMID 27838722.
- ^ a b Taylor F, Huffman MD, Macedo AF, Moore TH, Burke M, Davey Smith G, et al. (January 2013). "Statins for the primary prevention of cardiovascular disease". The Cochrane Database of Systematic Reviews. 2013 (1): CD004816. doi:10.1002/14651858.cd004816.pub5. PMC 6481400. PMID 23440795.
- ^ Pisaniello AD, Scherer DJ, Kataoka Y, Nicholls SJ (February 2015). "Ongoing challenges for pharmacotherapy for dyslipidemia". Expert Opinion on Pharmacotherapy. 16 (3): 347–356. doi:10.1517/14656566.2014.986094. PMID 25476544. S2CID 539314.
- ^ Lebenthal Y, Horvath A, Dziechciarz P, Szajewska H, Shamir R (September 2010). "Are treatment targets for hypercholesterolemia evidence based? Systematic review and meta-analysis of randomised controlled trials". Archives of Disease in Childhood. 95 (9): 673–680. doi:10.1136/adc.2008.157024. PMID 20515970. S2CID 24263653.
- ^ a b c National Institute for Health and Clinical Excellence. Clinical guideline 67: Lipid modification. London, 2008.
- ^ Grundy SM, Cleeman JI, Merz CN, Brewer HB, Clark LT, Hunninghake DB, et al. (August 2004). "Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines". Journal of the American College of Cardiology. 44 (3): 720–732. doi:10.1016/j.jacc.2004.07.001. PMID 15358046. S2CID 54525085.
- ^ Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. (June 2019). "2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines". Circulation. 139 (25): e1046–e1081. doi:10.1161/CIR.0000000000000624. PMID 30565953.
- ^ National Institute for Health and Clinical Excellence (18 July 2014). "Cardiovascular disease: risk assessment and reduction, including lipid modification". NICE. Retrieved 27 May 2019.
- ^ a b c d AMDA – The Society for Post-Acute and Long-Term Care Medicine (February 2014), "Ten Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, AMDA – The Society for Post-Acute and Long-Term Care Medicine, retrieved 20 April 2015
- ^ Snow V, Aronson MD, Hornbake ER, Mottur-Pilson C, Weiss KB (April 2004). "Lipid control in the management of type 2 diabetes mellitus: a clinical practice guideline from the American College of Physicians". Annals of Internal Medicine. 140 (8): 644–649. doi:10.7326/0003-4819-140-8-200404200-00012. PMID 15096336. S2CID 6744974.
- ^ Vijan S, Hayward RA (April 2004). "Pharmacologic lipid-lowering therapy in type 2 diabetes mellitus: background paper for the American College of Physicians". Annals of Internal Medicine. 140 (8): 650–658. doi:10.7326/0003-4819-140-8-200404200-00013. PMID 15096337. S2CID 25448635.
- ^ Barnes PM, Powell-Griner E, McFann K, Nahin RL (May 2004). "Complementary and alternative medicine use among adults: United States, 2002". Advance Data. 343 (343): 1–19. PMID 15188733.
- ^ Liu ZL, Liu JP, Zhang AL, Wu Q, Ruan Y, Lewith G, Visconte D, et al. (Cochrane Metabolic and Endocrine Disorders Group) (July 2011). "Chinese herbal medicines for hypercholesterolemia". The Cochrane Database of Systematic Reviews (7): CD008305. doi:10.1002/14651858.CD008305.pub2. PMC 3402023. PMID 21735427.
- ^ Demonty I, Ras RT, van der Knaap HC, Duchateau GS, Meijer L, Zock PL, et al. (February 2009). "Continuous dose-response relationship of the LDL-cholesterol-lowering effect of phytosterol intake". The Journal of Nutrition. 139 (2): 271–284. doi:10.3945/jn.108.095125. PMID 19091798.
- ^ Weingärtner O, Böhm M, Laufs U (February 2009). "Controversial role of plant sterol esters in the management of hypercholesterolaemia". European Heart Journal. 30 (4): 404–409. doi:10.1093/eurheartj/ehn580. PMC 2642922. PMID 19158117.
- ^ Carrol, Margaret (April 2012). "Total and High-density Lipoprotein Cholesterol in Adults: National Health and Nutrition Examination Survey, 2009–2010" (PDF). CDC.
- ^ Van Craeyveld E, Jacobs F, Gordts SC, De Geest B (2011). "Gene therapy for familial hypercholesterolemia". Current Pharmaceutical Design. 17 (24): 2575–2591. doi:10.2174/138161211797247550. PMID 21774774.
- ^ Al-Allaf FA, Coutelle C, Waddington SN, David AL, Harbottle R, Themis M (December 2010). "LDLR-Gene therapy for familial hypercholesterolaemia: problems, progress, and perspectives". International Archives of Medicine. 3: 36. doi:10.1186/1755-7682-3-36. PMC 3016243. PMID 21144047.

